Abstract
Purpose
Obstructive sleep apnea (OSA) is a prevalent and multifaceted disease. To date, the presence and severity of objectively identified comorbidities and their association with specific OSA phenotypes, CPAP adherence, and survival remain to be elucidated. The aim of this study is to cluster patients with OSA based on 10 clinically important objectively identified comorbidities, and to characterize the comorbidity clusters in terms of clinical and polysomnographic characteristics, CPAP adherence, and survival.
Study design and methods
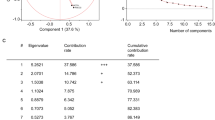
Seven hundred ten consecutive patients starting CPAP for moderate-to-severe OSA were included. Comorbidities were based on generally accepted cutoffs identified in the peer-reviewed literature. Self-organizing maps were used to order patients based on presence and severity of their comorbidities and to generate clusters.
Results
The majority of patients were men (80%). They were generally middle-aged (52 years) and obese (BMI: 31.5 kg/m2). Mean apnea-hypopnea index (AHI) was 41 ± 20 per h of sleep. More than 94% of the patients had one or more comorbidities with arterial hypertension, dyslipidemia, and obesity being the most prevalent. Nine comorbidity clusters were identified. The clinical relevance of these comorbidity clusters was highlighted by the difference in symptoms, PSG parameters, and cardiovascular risk. Also, differences in CPAP adherence, improvements in ESS, and long-term survival were present between the clusters.
Conclusion
Comorbidity prevalence in patients with OSA is high, and different comorbidity clusters, demonstrating differences in cardiovascular risk, CPAP adherence, and survival, can be identified. These results further substantiate the need for a comprehensive assessment of patients with OSA beyond the AHI.





Similar content being viewed by others
References
Lévy P, Kohler M, McNicholas WT et al (2015) Obstructive sleep apnoea syndrome. Nat Rev Dis Prim 1:15015. https://doi.org/10.1038/nrdp.2015.15
McNicholas WT, Bassetti CL, Ferini-Strambi L et al (2018) Challenges in obstructive sleep apnoea. Lancet Respir Med 6:170–172. https://doi.org/10.1016/S2213-2600(18)30059-6
Kendzerska T, Gershon AS, Hawker G et al (2014) Obstructive sleep apnea and risk of cardiovascular events and all-cause mortality: a decade-long historical cohort study. PLoS Med 11:e1001599. https://doi.org/10.1371/journal.pmed.1001599
Martínez-García M-A, Capote F, Campos-Rodríguez F et al (2013) Effect of CPAP on blood pressure in patients with obstructive sleep apnea and resistant hypertension: the HIPARCO randomized clinical trial. JAMA 310:2407–2415. https://doi.org/10.1001/jama.2013.281250
Zinchuk AV, Jeon S, Koo BB et al (2018) Polysomnographic phenotypes and their cardiovascular implications in obstructive sleep apnoea. Thorax 73:472–480. https://doi.org/10.1136/thoraxjnl-2017-210431
Bailly S, Destors M, Grillet Y et al (2016) Obstructive sleep apnea: a cluster analysis at time of diagnosis. PLoS ONE 11:e0157318. https://doi.org/10.1371/journal.pone.0157318
Sutherland K, Kairaitis K, Yee BJ, Cistulli PA (2018) From CPAP to tailored therapy for obstructive sleep apnoea. Multidiscip Respir Med 13:44. https://doi.org/10.1186/s40248-018-0157-0
Agusti A, Bel E, Thomas M et al (2016) Treatable traits: toward precision medicine of chronic airway diseases. Eur Respir J 47:410–419. https://doi.org/10.1183/13993003.01359-2015
Ye L, Pien GW, Ratcliffe SJ et al (2014) The different clinical faces of obstructive sleep apnoea: a cluster analysis. Eur Respir J 44:1600–1607. https://doi.org/10.1183/09031936.00032314
Vavougios GD, George DG, Pastaka C et al (2016) Phenotypes of comorbidity in OSAS patients: combining categorical principal component analysis with cluster analysis. J Sleep Res 25:31–38. https://doi.org/10.1111/jsr.12344
Gagnadoux F, Le Vaillant M, Paris A et al (2016) Relationship between OSA clinical phenotypes and CPAP treatment outcomes. Chest 149:288–290. https://doi.org/10.1016/j.chest.2015.09.032
Lacedonia D, Carpagnano GE, Sabato R et al (2016) Characterization of obstructive sleep apnea-hypopnea syndrome (OSA) population by means of cluster analysis. J Sleep Res 25:724–730. https://doi.org/10.1111/jsr.12429
Bailly S, Grote L, Hedner J et al (2020) Clusters of sleep apnoea phenotypes: a large pan-European study from the European Sleep Apnoea Database (ESADA). Respirology. https://doi.org/10.1111/resp.13969
Labarca G, Dreyse J, Salas C et al (2020) A clinic-based cluster analysis in patients with moderate-severe obstructive sleep apnea (OSA) in Chile. Sleep Med 73:16–22. https://doi.org/10.1016/j.sleep.2020.04.001
Triest FJJ, Franssen FME, Spruit MA et al (2015) Poor agreement between chart-based and objectively identified comorbidities of COPD. Eur Respir J 46:1492–1495. https://doi.org/10.1183/13993003.00667-2015
Augustin IML, Spruit MA, Franssen FME et al (2020) Incorporating comprehensive assessment parameters to better characterize and plan rehabilitation for persons with chronic obstructive pulmonary disease. J Am Med Dir Assoc 21:1986-1991.e3. https://doi.org/10.1016/j.jamda.2020.05.026
Spruit MA, Augustin IML, Vanfleteren LE et al (2015) Differential response to pulmonary rehabilitation in COPD: multidimensional profiling. Eur Respir J 46:1625–1635. https://doi.org/10.1183/13993003.00350-2015
Jennum P, Tønnesen P, Ibsen R, Kjellberg J (2017) Obstructive sleep apnea: effect of comorbidities and positive airway pressure on all-cause mortality. Sleep Med 36:62–66. https://doi.org/10.1016/j.sleep.2017.04.018
Marrone O, Lo Bue A, Salvaggio A et al (2013) Comorbidities and survival in obstructive sleep apnoea beyond the age of 50. Eur J Clin Invest 43:27–33. https://doi.org/10.1111/eci.12011
Bonsignore MR, Baiamonte P, Mazzuca E et al (2019) Obstructive sleep apnea and comorbidities: a dangerous liaison. Multidiscip Respir Med 14:8. https://doi.org/10.1186/s40248-019-0172-9
Kent BD, Grote L, Ryan S et al (2014) Diabetes mellitus prevalence and control in sleep-disordered breathing: the European Sleep Apnea Cohort (ESADA) study. Chest 146:982–990. https://doi.org/10.1378/chest.13-2403
Vanfleteren LEGW, Spruit MA, Groenen M et al (2013) Clusters of comorbidities based on validated objective measurements and systemic inflammation in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 187:728–735. https://doi.org/10.1164/rccm.201209-1665OC
Keenan BT, Kim J, Singh B, et al (2018) Recognizable clinical subtypes of obstructive sleep apnea across international sleep centers: a cluster analysis. Sleep 41. https://doi.org/10.1093/sleep/zsx214
Lustberg L, Reynolds CF (2000) Depression and insomnia: questions of cause and effect. Sleep Med Rev 4:253–262. https://doi.org/10.1053/smrv.1999.0075
McCarthy A, Wafford K, Shanks E et al (2016) REM sleep homeostasis in the absence of REM sleep: effects of antidepressants. Neuropharmacology 108:415–425. https://doi.org/10.1016/j.neuropharm.2016.04.047
Nigam G, Pathak C, Riaz M (2016) A systematic review of central sleep apnea in adult patients with chronic kidney disease. Sleep Breath 20:957–964. https://doi.org/10.1007/s11325-016-1317-0
Degache F, Sforza E, Dauphinot V et al (2013) Relation of central fat mass to obstructive sleep apnea in the elderly. Sleep 36:501–507. https://doi.org/10.5665/sleep.2532
Wallace DM, Sawyer AM, Shafazand S (2018) Comorbid insomnia symptoms predict lower 6-month adherence to CPAP in US veterans with obstructive sleep apnea. Sleep Breath 22:5–15. https://doi.org/10.1007/s11325-017-1605-3
Luyster FS, Buysse DJ, Strollo PJ (2010) Comorbid insomnia and obstructive sleep apnea: challenges for clinical practice and research. J Clin Sleep Med 6:196–204
Drager LF, Brunoni AR, Jenner R et al (2015) Effects of CPAP on body weight in patients with obstructive sleep apnoea: a meta-analysis of randomised trials. Thorax 70:258–264. https://doi.org/10.1136/thoraxjnl-2014-205361
Basoglu OK, Zou D, Tasbakan MS et al (2018) Change in weight and central obesity by positive airway pressure treatment in obstructive sleep apnea patients: longitudinal data from the ESADA cohort. J Sleep Res 27:e12705. https://doi.org/10.1111/jsr.12705
Yang K, Wu Y, Chen D et al (2020) The impact of lung function on extra-pulmonary diseases and all-cause mortality in US adult population with and without COPD. Clin Epidemiol 12:997–1005. https://doi.org/10.2147/CLEP.S270599
Chandra D, Gupta A, Fitzpatrick M et al (2019) Lung function, coronary artery disease, and mortality in HIV. Ann Am Thorac Soc 16:687–697. https://doi.org/10.1513/AnnalsATS.201807-460OC
Nakamura K, Kanzaki H, Okada A et al (2019) Independent prognostic value of pulmonary diffusing capacity in nonsmoking patients with chronic heart failure. Int Heart J 60:366–373. https://doi.org/10.1536/ihj.18-420
Stadler S, Mergenthaler N, Lange TJ (2019) The prognostic value of DLCO and pulmonary blood flow in patients with pulmonary hypertension. Pulm Circ 9:204589401989453. https://doi.org/10.1177/2045894019894531
Willis A, Davies M, Yates T, Khunti K (2012) Primary prevention of cardiovascular disease using validated risk scores: a systematic review. J R Soc Med 105:348–356. https://doi.org/10.1258/jrsm.2012.110193
BaHammam AS, Kendzerska T, Gupta R et al (2016) Comorbid depression in obstructive sleep apnea: an under-recognized association. Sleep Breath 20:447–456. https://doi.org/10.1007/s11325-015-1223-x
Levine CG, Weaver EM (2014) Functional comorbidity index in sleep apnea. Otolaryngol Head Neck Surg 150:494–500. https://doi.org/10.1177/0194599813518164
Pichel F, Zamarrón C, Magán F et al (2004) Health-related quality of life in patients with obstructive sleep apnea: effects of long-term positive airway pressure treatment. Respir Med 98:968–976. https://doi.org/10.1016/j.rmed.2004.03.009
Smith R, Ronald J, Delaive K et al (2002) What are obstructive sleep apnea patients being treated for prior to this diagnosis? Chest 121:164–172
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. This study was approved by the Ethical Committee of UZ Leuven (ML7962).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Testelmans, D., Spruit, M.A., Vrijsen, B. et al. Comorbidity clusters in patients with moderate-to-severe OSA. Sleep Breath 26, 195–204 (2022). https://doi.org/10.1007/s11325-021-02390-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02390-4